How GP Practices Can Ensure Cyber-Secure Telehealth Services
Learn effective ways to protect GP telehealth systems from data breaches, ransomware, and cyber risks with simple, actionable security practices.

The rise of telehealth in UK general practice has transformed patient care, enabling greater access to consultations and ongoing support without patients needing to leave their homes. However, with this digital transformation comes an urgent responsibilityprotecting sensitive health data against increasing cyber threats.
As GP practices continue to rely on virtual platforms for consultations, prescriptions, and records, cybersecurity becomes a non-negotiable priority. In this blog, we explore practical steps GP surgeries can take to ensure that their telehealth services are secure, reliable, and compliant with UK data protection laws.
The Growing Importance of Telehealth in General Practice
Telehealth has moved from being a convenience to a necessity in todays healthcare system. After the pandemic accelerated digital adoption, many GP surgeries now rely on video consultations, online booking systems, and electronic prescriptions.
This shift has allowed practices to better manage workloads, serve patients in rural or underserved areas, and reduce face-to-face contact when unnecessary. The NHS continues to support digital-first healthcare initiatives, making it clear that telehealth is here to stay.
However, increased online interaction also opens doors to cybercriminals, data breaches, and system vulnerabilities. These threats are not hypothetical; they are real, growing, and dangerous.
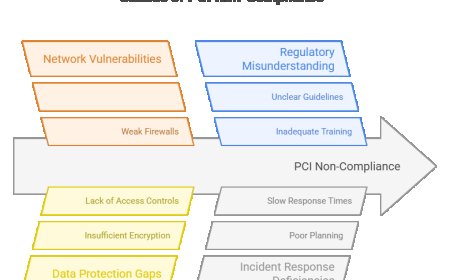
Common Cyber Threats Facing GP Telehealth Platforms
GP practices, despite being small to medium-sized organisations, are attractive targets for cybercriminals due to the sensitive nature of the data they hold. Here are some of the most common threats:
- Phishing Attacks: Fraudulent emails or messages aimed at tricking staff into revealing login credentials.
- Ransomware: Malicious software that locks systems or data until a ransom is paid.
- Unsecured Video Calls: If not properly encrypted, patient-doctor conversations can be intercepted.
- Outdated Software: Unsupported or unpatched software creates vulnerabilities that attackers can exploit.
These risks can disrupt service delivery, compromise patient confidentiality, and lead to hefty fines under data protection laws.
Core Cybersecurity Principles for GP Telehealth
To combat these risks, GP practices should build cybersecurity into the foundation of their telehealth services. The following core principles are essential:
- End-to-End Encryption: Ensures all communication between patients and healthcare professionals remains private and secure.
- Secure Authentication: Use of strong passwords and two-factor authentication for accessing patient records or video consultation platforms.
- Device Security: Only approved, secure devices should be used for remote consultations or data access.
- Regular Software Updates: Keep all systems and applications up to date to eliminate known security flaws.
- Access Controls: Staff should only have access to the data they need for their role. This limits potential exposure in case of a breach.
Practices should work closely with trusted providers ofhealthcare IT consultingto design and maintain secure systems tailored to their needs.
Checklist for Securing a Telehealth Service
A clear, practical checklist can help practices stay on top of key cybersecurity responsibilities. Heres a summary in table format:
|
Security Measure |
Purpose |
Implementation Tip |
|
End-to-End Encryption |
Protects consultations from unauthorised access |
Use NHS-approved video tools |
|
Two-Factor Authentication |
Adds extra layer of security to logins |
Set up via NHSmail or similar platforms |
|
Cybersecurity Training for Staff |
Reduces risk of human error |
Conduct annual awareness sessions |
|
Regular Software Updates |
Fixes bugs and vulnerabilities |
Enable auto-updates on all devices |
|
Secure Wi-Fi/VPN Use |
Protects data in transit |
Use NHS Digital-approved virtual networks |
|
Backup and Recovery Solutions |
Ensures resilience against ransomware |
Backup data to secure, encrypted cloud servers |
Role of Staff Training and Cyber Hygiene
Technology alone cannot protect a GP practice from cyber threats. Human error remains one of the biggest cybersecurity risks. Thats why staff training is critical.
All team memberswhether clinical, administrative or technicalshould be trained to:
- Recognise phishing emails and suspicious activity.
- Follow secure password protocols.
- Use only approved devices for patient interactions.
- Report potential security incidents immediately.
Some practices also run simulated phishing attacks to test staff responses and improve awareness. Encouraging a culture of cyber hygiene ensures that everyone in the practice takes responsibility for data protection.
Choosing the Right Telehealth Platforms
Not all telehealth tools are created equal. GP practices should choose platforms that are built with security in mind and meet NHS Digital standards.
When selecting a provider, make sure they are:
- Cyber Essentials certified.
- Transparent about where and how data is stored.
- Using industry-standard encryption protocols.
- Capable of providing data processing agreements (DPAs).
Ask vendors questions such as:
- Where are your servers located?
- What encryption do you use?
- How do you handle a breach?
Working with an experiencedIT consultancy Londoncan help navigate these decisions and ensure your telehealth infrastructure is both secure and scalable.
Compliance with UK Regulations
GP practices are legally responsible for the safety of patient data. Ensuring your telehealth service is compliant with UK law is essential.
- GDPR: The General Data Protection Regulation requires that personal data is processed securely, fairly, and lawfully.
- NHS DSPT: The Data Security and Protection Toolkit is a mandatory self-assessment that all practices must complete annually.
- ICO Guidance: Follow the Information Commissioners Office guidelines for secure data processing and reporting breaches.
Non-compliance can lead to serious consequences, including financial penalties and loss of patient trust.

Example: A Wake-Up Call
In one UK practice, a staff member clicked on a phishing link disguised as an NHS email. The result was a ransomware attack that locked access to the practice's patient records for two days. While no data was leaked, the disruption to services was significant.
After the incident, the practice partnered with a healthcare IT consulting provider to improve security, train staff, and install more robust monitoring tools. They have since avoided further incidents and now serve as a model for neighbouring practices.
Conclusion: Make Cybersecurity Part of Your Practice Culture
Cybersecurity is no longer just a technical concernits a patient safety priority. With telehealth becoming vital for GP practices, robust security is essential. From encryption and compliance to staff training and platform selection, every aspect must be addressed.
Renaissance Computer Services Limited supports GP practices across the UK in building secure, efficient telehealth systems. As a trusted IT consultancy in London, we understand the unique demands of healthcare.
Dont wait for a breachreview your current systems, train your team, and work with experts who truly understand healthcare IT. The future of care is digitalensure its also safe and secure.